Informasjon om en nyhet med tittelen International Research Partnership Looks to Improve how ACL Revision Outcomes are Predicted and Treated
International Research Partnership Looks to Improve how ACL Revision Outcomes are Predicted and Treated
Introduksjon
Author: Brianna Vitands, Communications/Web Specialist, Department of Orthopedic Surgery | OCTOBER 26, 2020
The text and photo is from the following website: https://bit.ly/3kDVTYt
The anterior cruciate ligament (ACL) is a vital knee stabilizer responsible for maintaining balance and function. ACL injuries are common and can cause prolonged pain, instability and an increased risk of post-traumatic osteoarthritis. Patient-specific variables, including age, graft choice and fixation method, have been shown to increase the likelihood of a surgical reconstruction failure, which can lead to additional pain and immobility. With so many variables to consider, accurately predicting a patient’s expected outcome is critical.
Kyle Martin, MD, an assistant professor in the Department of Orthopedic Surgery in the University of Minnesota Medical School, believes that machine learning could help predict a patient’s individualized outcomes more accurately and ultimately change how physicians choose to treat them. With the primary goal of creating an in-clinic calculator that physicians can use to predict the risk of ACL reconstruction failure at a patient-specific level, Dr. Martin’s project, “Robust predictive model for patient outcome following anterior cruciate ligament surgery (ACL) using the Norwegian Knee Ligament Registry (NLKR) and Machine Learning,” recently received grant funding through the Norwegian Centennial Chair Program.
“The funding represents a partnership between the Norwegian University of Life Sciences, University of Oslo and University of Minnesota Medical School to foster and encourage transatlantic collaboration on research studies,” Dr. Martin said.
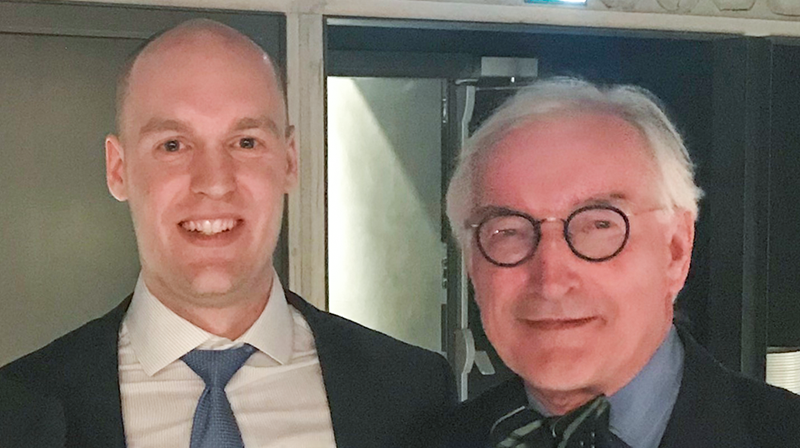
The international partnership was serendipitous. Prior to starting his Minnesota practice, Dr. Martin completed a sports medicine fellowship at the Oslo University Hospital in Norway. There, he trained under the tutelage of Lars Engebretsen, MD, PhD, a professor at the University of Oslo, former chair of the Orthopedic Clinic at the University of Oslo and chair of the Oslo Sports Trauma Research Center. Dr. Engebretsen has Minnesota connections himself, having worked as an associate professor in the U of M Medical School’s Department of Orthopedic Surgery from 1991 to 1996.
“It was a coincidence that Dr. Martin ended up in Minnesota, because he had been working with us in Oslo on the Norwegian ACL registry data for the last year,” Dr. Engebretsen said.
When Dr. Martin arrived at the Medical School, he partnered with biostatistician Julian Wolfson, PhD, an associate professor in the School of Public Health’s Division of Biostatistics. They began planning an advanced statistical analysis of the NKLR data using machine learning. With over 25,000 patients, the registry contains patient-specific variables, intraoperative surgical details and patient-reported outcomes, both pre- and post-operatively at two, five and 10 years after the procedure.
“From previous registry analysis, we know that certain factors, such as graft choice (i.e. hamstring versus patellar tendon graft) have a different revision rate,” Dr. Martin explained. “Other factors, including age, weight and sex, may also contribute to higher risk, but those are just some of the known variables. Through our analysis, we may identify more.”
Two to four studies will be funded through the grant, which provides $150,000 over the course of two years. The first study will look at the risk of ACL reconstruction failure, defined as having a revision surgery. Dr. Martin and his team want to find out which variables are associated with revision risk and how accurately the algorithm can use these identified factors to make a prediction.
“Relatively speaking, we’re pretty good at predicting who is considered high and low-risk given the general population, but we don’t know how much weight to put on each variable or how to quantify risk of failure at a patient-specific level,” Dr. Martin said. “The goal is to use all of the information in the database, not just the risk factors we know, to provide customized estimates that are more precise.”
The results of this project will be used to develop an in-clinic calculator that physicians can use to input individual patient variables and calculate their specific risk of ACL reconstruction failure.
“Some of the factors are modifiable, so the in-clinic calculator could help guide surgical discussion of the options from a risk perspective,” Dr. Martin explained. “It will help physicians have more confidence in their recommendations surrounding surgical decision-making.”
Databases like the NKLR are rare in the United States. Kaiser Permanente, an insurance company, has its own private ACL reconstruction registry with voluntary patient enrollment. The National Collegiate Athletic Association (NCAA) Injury Surveillance Program maintains a database to track and analyze injuries resulting from participation in collegiate athletics, including ACL reconstruction. These athletes, however, are a specific group of patients that are not representative of the general population, and results from machine learning analysis of the data wouldn’t necessarily apply to the average person.
“Using a U.S. national registry to do this project isn’t really feasible due to our health system,” Dr. Martin said. “The system in Norway lends itself to registry creation, and they have an impressive capture rate of ACL reconstructions.”
The NKLR includes the entire country of Norway, whose population is generally willing to contribute data, according to Dr. Engebretsen. While roughly 90 percent of Norway’s healthcare is government-based, private practice physicians are typically compliant in adding their patients as well. While the NKLR data is robust, Dr. Engebretsen notes that the School of Public Health’s Division of Biostatistics has more experience applying machine learning.
“It’s an international project,” Dr. Engebretsen said. “It makes use of the data we have, which can’t be obtained in the U.S., and the technical work of the biostatisticians, which couldn’t be done here, so it’s very beneficial for both parties.”

